Referral of SMA to a Neurologist
Early recognition and referral of a patient with suspected spinal muscular atrophy (SMA) to a neurologist.
Episodes in this series
Garey H. Noritz, MD: Hello, and thank you for joining this NeurologyLive® Cure Connections® program titled “Cure SMA: Evaluation of SMA in the Era of Telehealth.”
Today we’re going to discuss the diagnosis of SMA [spinal muscular atrophy], including the virtual visit during COVID-19 [coronavirus disease 2019]. I’m Dr Garey Noritz, a pediatrician from Nationwide Children’s Hospital in Columbus, Ohio. Joining me today is Dr Diana Castro, a pediatric neurologist at Children’s Health of UT Southwestern in Dallas, Texas.
Thanks so much for joining us. Let’s begin. Dr Castro, can you tell us a little bit about your practice?
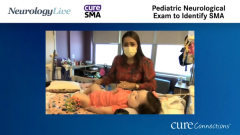
Diana Castro, MD: Sure. Thank you so much for the invitation. We’re actually one of the largest neuromuscular practices. We have about 150 patients with spinal muscular atrophy, divided in terms of types 1, 2, and 3. Most of the patients are getting therapy. I only see neuromuscular patients, and I work very closely with a pulmonologist, gastroenterologist, and orthopedic surgeons. Those are the main people with other specialties who help me. I also have a nurse coordinator, PT [physical therapist], OT [occupational therapist], and nutritionist. I’m blessed with my practice. I cannot complain.
Garey H. Noritz, MD: It’s so great to have a team to help you with patients who have a disease that is this complicated, and I’m sure the families appreciate coming to one place and getting a lot of their problems addressed at the same time. But one of the problems is getting them to you in the first place, right? How do patients get the diagnosis of SMA, and how do they then make it to a neuromuscular center?
Diana Castro, MD: Unfortunately, we don’t have newborn screening yet here in Texas. We’re hoping that we’ll get it in 2021. Right now we’re mainly relying on the clinical diagnosis and the referrals we get from pediatricians, family physicians, and sometimes physical therapists as well. I think it’s great because they’re also getting educated and informed about treatments that can be given. I try to be very open with my colleagues, pediatricians, and so on to try to have a direct line of communication. They will have my cell phone number, or they will send the referral and email, or call me to let me know that they’re worried about a patient with spinal muscular atrophy with low muscle tone.
If that’s the case, those patients come to me or my colleague right away. We try to see the patient on the same day or the day after but never later than that. For us, it’s almost like an emergency. We bring the patients in really quickly. We have also been working with our schedulers to discuss or have key words in the referrals that they will see and then send the referral directly to us. If they see hypotonia, absent reflexes, CK [creatine kinase], or whatever is the case, they will come directly to us, and they will keep that long process of review.
Garey H. Noritz, MD: Thank you for watching this NeurologyLive® Cure Connections® program. If you enjoyed the content, please subscribe to our e-newsletters to receive upcoming programs and other great content right in your inbox.
Transcript Edited for Clarity
Newsletter
Keep your finger on the pulse of neurology—subscribe to NeurologyLive for expert interviews, new data, and breakthrough treatment updates.